When it comes to healthcare careers, many immediately think about doctors and nurses. However, there are many other career options within the industry. In addition to job security, these professions also offer generous salaries. Whether you’re in the medical staffing industry, ready to grow or launch your own healthcare staffing company, or deciding on a healthcare career specialty, consider these growing fields.
Pharmacist: Aside from dispensing prescription medications, pharmacists provide valuable advice pertaining to prescription drugs, as well as how to safely use them. Salary=$117,000, Projected job growth=25 %
Podiatrist: Podiatrists help patients with foot, ankle, and lower leg problems. In addition to providing diagnoses for illnesses, podiatrists also treat injuries and provide surgical care for patients. Salary=$116,000, Projected job growth=20%
Optometrist: Specializing in eye exams, optometrists perform routine checks to detect vision problems and diseases. Optometrists also write prescriptions for eyeglasses or contact lenses. Salary=$98,000, Projected job growth=33%
Physical Therapist: In addition to pain management, physical therapists help patients with injuries or illnesses improve their movement. Salary=$80,000, Projected job growth=39%
Occupational Therapist: Occupational therapists help patients suffering from illnesses, injuries, or disabilities by introducing therapeutic techniques and equipment that can help improve the skills necessary for everyday living and working. Salary=$75,000, Projected job growth=33%
Speech Pathologist: Speech-language pathologists provide treatment and diagnoses for communication and swallowing disorders. Salary=$70,000, Projected job growth=23%
Chiropractor: Chiropractors offer treatment for patients encountering health problems with bones, muscles, ligaments, and tendons. By using spinal manipulation and other treatments, chiropractors also help treat patients’ back or neck pain. Salary=$66,000, Projected job growth=28%
Respiratory Therapist: Patients suffering from breathing problems, such as asthma or emphysema, seek care from respiratory therapists. Additionally, respiratory therapists offer urgent care to patients encountering a stroke, heart attack, or shock. Salary=$56,000, Projected job growth=28%
Laboratory Technician: Laboratory technicians collect samples from patients and perform tests to further examine tissue, body fluids, and other substances. Salary=$36,950, Projected job growth=15%
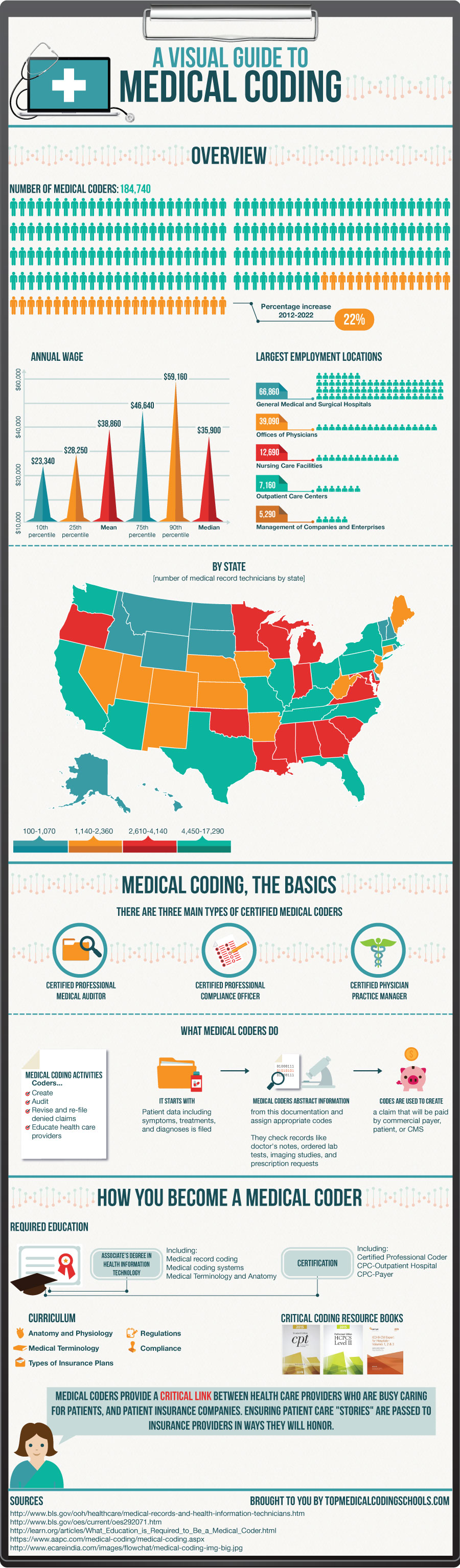
Medical Records Technician: Aside from managing and organizing health information data, medical records technicians make sure that the information is accurate, secure, and readily accessible via paper and electronic systems. Salary=$35,000, Projected job growth =21%
Thanks to the implementation of Obamacare, healthcare jobs are poised to experience massive growth as more people seek services. For more information on the hottest healthcare careers for 2014, visit the Bureau of Labor Services Occupational Outlook Handbook for healthcare.